In this section, we will cover:
What comprises shared decision making
How shared decision making improves health equity
Why it is good for individuals and providers to partner when making care decisions
What digital health tools help individuals and providers collaborate
How individuals could be involved in co-design of the digital health tools they use
Shared decision making is a process that digital health tools can facilitate. It is not a technology. The United Kingdom’s National Health Service explained “Shared decision-making ensures that individuals are supported to make decisions that are right for them. It’s a collaborative process through which a clinician supports an individual to reach a decision about their treatment. The conversation brings together:
- the clinician’s expertise, such as treatment options, evidence, risks and benefits
- what the individual knows best: their preferences, personal circumstances, goals, values and beliefs.” (101)
Literature on shared decision making is available ranging from broad populations to specialty care. The Kingdom of Saudi Arabia cited examples of both. A study of individuals aged 18 and older, The OPTION Scale: Measuring Patients’ Perceptions of Shared Decision-Making in the Kingdom of Saudi Arabia, concludes, “Generally, the study results confirmed that shared decision-making in the Saudi health system includes significant patient involvement. Interventions that enhance the culture of shared decision-making in Saudi Arabia are necessary to ensure better adherence to treatment plans and thus better health outcomes.” (102) The doctoral thesis Patients as active partners in decision-making: A qualitative exploration of the perspectives of people with T2D and their clinicians in a diabetes centre in Saudi Arabia, states that the study contributes original knowledge “by exploring the views and experiences of both users and providers of diabetes care about patient involvement in decision-making.” (103) Although these studies are country-specific, they confirm the importance of shared decision making.
One example of a shared decision-making process is described in The SHARE Approach: A Model for Shared Decision Making – Fact Sheet, a five-step process described by the United States of America’s Agency for Healthcare Research and Quality (AHRQ). Many resources, including workshop curriculum, tools, webinars, and success stories, are available on the SHARE Approach website to help you implement shared decision making in practice. (104)

Are Individuals and Caregivers Regarded as Partners in Care?
A partnership requires two persons or entities who agree to work together. For shared decision making the persons are:
- An individual or caregiver who wants to collaborate (engage) with their provider as more than a follower and
- A provider who wants to engage with individuals/caregivers and incorporate individuals and/or caregivers into the decision-making process.
Shared decision making is key to improving health equity.The National Academy of Medicine published a paper that noted, “Achieving health equity requires flipping the traditional institutional approach to delivering health care that positions providers as the sole experts and deprioritizes the experiences of a diverse population. We must leverage all talents, including those of individuals, families, and communities who have a wealth of knowledge to share and should be included as equal partners, to help achieve population health with health equity at its core. To achieve such a transformation, inclusion of people from a diverse background, with full transparency, is essential.” (105)
Individual-centered metrics such as Patient-Reported Outcome Measures (PROMs) and PREMs can be used to incorporate individual perspectives into shared decision making. Examples of PROMs are ratings of individuals’ pain, physical functioning, and psychological well-being. Examples of PREMs are individuals’ experiences with healthcare, such as waiting times and communication with healthcare providers.
PROMs and PREMs can also be used as the basis for cross-country studies of patient populations, as they are in the OECD Patient-Reported Indicator Surveys (PaRIS). This survey is the largest international study of adult patients in primary care to-date, with 20 countries participating in the first survey cycle in 2023-2024. The analysis of the complete dataset will merge characteristics and perspectives of individuals and providers collected through surveys with the extensive dataset of health systems indicators regularly gathered by the OECD.
The OECD PaRIS initiative is the first of its kind and will provide much-needed insights into the outcomes and experiences of primary care individuals through gathering evidence on access to healthcare, including digital and remote interactions, waiting times, quality of life, pain, physical functioning, psychological well-being, and more. The aim is to produce novel policy insights on health system performance and access, focusing on the aspects that matter most for individuals. The OECD will release a comprehensive flagship report in late 2024 based on data from over 1,500 primary care providers and over 120,000 individuals across OECD countries. The report will contain in-depth analyses, including variation across and within countries and population groups, exploring the rich datasets that are currently being collected. (84)
While OECD is studying primary care individuals, the DIALOG+ project in Europe is an example of studying the effects of individual and provider partnership in specialty care using PROMs and PREMs. SHARE focuses on a collaborative process and DIALOG+ focuses on using measurements of individual outcomes and experiences to inform the individual-provider relationship. Sweden shares their study on the Dialog+ project that was developed to make routine individual-clinician meetings therapeutically effective.
Sweden | From Around the Globe
Study the Effects of Partnership in Psychiatry
To demonstrate the international impact that effective individual engagement can deliver, Sweden referenced the multi-year project DIALOG+ +. Originally developed in the United Kingdom by the Queen Mary University of London and the East London NHS Foundation Trust, the Dialog+ project is the first approach that has been specifically developed to make routine individual-clinician meetings therapeutically effective. It is based on quality-of-life research, concepts of individual-centered communication, IT developments, and components of solution-focused therapy. It is also supported by an app. Research studies in different mental health services and multiple countries have shown that using Dialog+ can improve individuals’ quality of life. (106) Individual feedback supports both individuals and therapists in visits and uses PROMs and PREMs as care planning tools.
What Digital Health Tools Help Individuals and Providers Collaborate?
Technology can facilitate the shared decision-making process when it helps individuals and providers work together as partners. Even digital health tools not directly focused on shared decision making can support it indirectly as explained in the Kingdom of Saudi Arabia member story.
Kingdom of Saudi Arabia | From Around the Globe
Digital Health Tools and Services to Facilitate Collaboration
Partnerships between individuals and providers is the unifying theme the Kingdom of Saudi Arabia highlights in their digital health tools below:
- EHRs enable individuals to review their health information, access educational information, and actively participate in discussions with their providers.
- Individual portals empower individuals to engage in their care and communicate with their providers.
- Telehealth and telemedicine services enable individuals to have remote consultations with their providers via video conferencing or secure messaging.
- Mobile health apps such as medication trackers, fitness apps, and symptom diaries all help individuals connect with providers to support informed decisions.
- The National Platform for Health and Insurance Exchange Services (NPHIES), the Kingdom of Saudi Arabia’s health information exchange, improves care coordination and ensures all providers have access to up-to-date individual information.
- Qareboon, an integrated library of text materials, infographics and videos, supports psychological counseling services for individuals.
- Wearable devices such as smart watches are commonly used to collect data like heart rate, activity levels, and sleep patterns. They enable individuals to monitor their health and share device data with their providers.
- Secure messaging apps and chatbots allow individuals to ask questions, seek guidance, and receive information promptly from their providers.
While digital health tools that have individual information in them can aid in shared decision making, the use of AI in digital health tools has also gained interest in the health community.
While digital health tools that have individual information in them can aid in shared decision making, the use of AI in digital health tools has also gained interest in the health community. HealthAI (formerly known as I-DAIR), an international organization that advances the governance and regulation of artificial intelligence, discussing AI as it relates to individual reported outcome monitoring and noted that: “Nowadays, relatively subjective criteria, such as trustworthiness, are gaining ground and becoming a prerequisite to scale future AI/data use in health… The e-PROM project is a first step to develop consensus on a shift in focus from technical accuracy towards human-centered evaluation of digital health and AI solutions, and stimulate the development of a roadmap for the development of a new generation of human-centered benchmarks combining qualitative and quantitative methodologies. … In its current developments, I-DAIR has begun work on integrating electronic Patient Reported Outcome Monitoring (ePROM) into clinical practice in the oncology setting (India) as well as the neurological setting (Tunisia).” (107) PROMs and PREMs will help advance more individual-centered care.
In the United Kingdom, a dialogue was conducted on how the public feel decisions should be made about access to their personal health data for AI research.
United Kingdom | From Around the Globe
Individual and Public Involvement in Data Stewardship
The NHS AI Lab and Sciencewise co-commissioned a deliberative dialogue on how decisions should be made about accessing health data for AI research and development. The aim of the dialogue was to understand participants’ attitudes towards different approaches to data stewardship, including options for involving individuals and the public more deeply as part of the decision-making process. The findings surfaced principles for making decisions about data access, for example that ‘participants often suggested that a combination of complementary approaches should be used, given that no single approach was seen as perfect’ and ultimately informed the proposal of different data stewardship models, which will be further explored as policies for Secure Data Environments are developed. (108)
Do Individuals Help Co-Design Digital Health Tools?
Individuals and caregivers can help co-design digital health tools at local, regional, or national levels. The Academic Emergency Medicine’s Patient Engagement and the Design of Digital Health notes “Despite the rhetoric and hope for digital health, however, patients are not using the tools as much as they could. Typical medical or fitness apps have a 90-day user retention rate of only 27% to 30%… Existing digital health tools generally fail to address the issues that matter to patients (and doctors) and fail to feel relatable. To create relevant, usable, and effective digital health, it is critical to increase patients’ involvement in the design of technologic tools…In patient-led design, it is patients themselves who determine the focus of an intervention: what a digital health tool should focus on and how it should do so…Patient-designed, patient-centered digital health tools are more likely to be bridge the gap between existing products and populations who would most benefit and to realize the promise of digital health.” (109) GDHP members’ experiences reinforce the paper’s recommendations about the importance of individual and caregiver involvement in the co-design of digital health systems such as portals and mobile health apps. GDHP members’ experiences reinforce the paper’s recommendations about the importance of individual and caregiver involvement in co-design of digital health systems such as portals and mobile health apps.
Brazil | From Around the Globe
Build Knowledge and Trust through Individual Assistance in Constructing Digital Health Systems
In its National Digital Health Strategy, the Brazil Ministry of Health acknowledges a lack of knowledge and trust among public and private sector partners for healthcare equipment, services, and products. To bridge the gap in knowledge and trust, the strategy defines a priority, “The User as Protagonist,” which means leveraging “engagement of patients and citizens to promote the adoption of healthy habits and the management of their health, their family and their community, in addition to assisting in the construction of the information systems they will use.” (55) Brazil has also been strengthening citizen engagement through a series of actions such as the ethnic-racial equity workshop for Sistema Único de Saúde (SUS) Digital, the mini-app Equity SUS, the requirement for the race-color field in health information systems, and the Menstrual Dignity Initiative.
There is a wide range of opportunities for individuals to assist in the construction (co-design) of the information systems they will use. For example, there are systems containing various digital health tools intended for the entire population to use, such as Poland’s national portal.
Poland | From Around the Globe
Individual Involvement in National Portal Design
Individuals were involved in the design of Poland’s national portal through consultation in the early stages of its design and through user experience (UX) tests.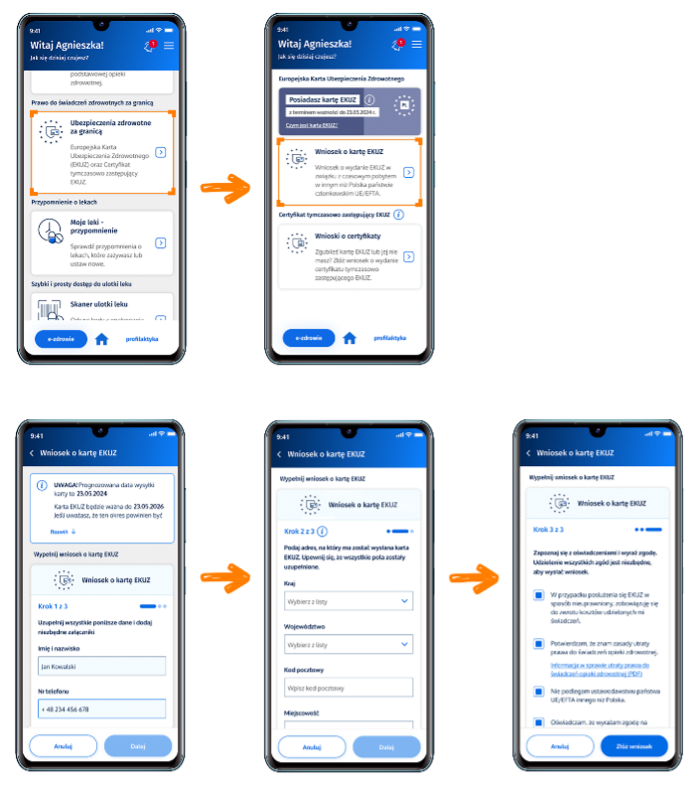
In other cases, individual co-design may focus narrowly on specialized tools for a subset of the population, such as a Korean app for people who are differently abled and their caregivers.
Republic of Korea | From Around the Globe
Co-Design of an App for the Disabled and their Caregivers
To develop a Lifelog data management app for people with different abilities, a Co-Creation Workshop was held with people with different abilities and their caregivers to engage them in the app’s design. The workshop includes brainstorming and mind map design, persona and scenario derivation, user requirements derivation, and design of the user interface and user experience. (110)
Furthermore, co-design may occur at the country-wide level. Ireland has a formal structure to keep individuals engaged with the government in the design and delivery of health services.
Ireland | From Around the Globe
A National Patient Forum
Ireland’s Health Service Executive runs a National Patient Forum including individuals, family members, caregivers, representatives of advocacy groups, disability organizations and Patients for Patient Safety Ireland. It seeks input from individuals and service users in a range of issues, including the design and delivery of services. They use techniques such as:
- Presentations to the forum members, followed by question-and-answer sessions;
- Focus group discussions;
- Workshops; and
- Questionnaires and surveys. (111)
Shared Decision Making Recap
Shared decision-making tools for success include these actions you may want to consider:
- Use a shared decision-making process to bring individuals and clinicians together as partners in the individual’s care;
- Consider the potential model for shared decision making (e.g., the SHARE approach);
- Include individuals from diverse backgrounds to help advance your country’s health equity efforts;
- Use PREMs and PROMs as quantitative tools to inform shared decision making;
- Involve individuals and caregivers in co-designing digital health tools, especially those they are intended to use, such as an individual portal; and
- Include individuals and caregivers to co-design your health services and programs.

